New guidance published to help GPs interpret Lateral Flow Device test results
2 July 2021
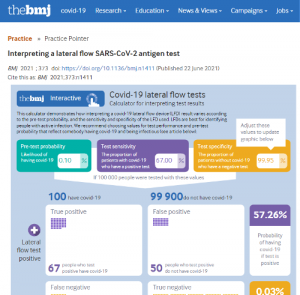
New guidance for GPs and other health professionals on how to interpret and communicate results from Lateral Flow Device (LFDs) tests based on the current understanding of the tests’ performance is published in the BMJ. Researchers from the Universities of Bristol, Cambridge, and Trinity College Dublin have devised a calculator which aims to help doctors, who are increasingly asked by patients what they should do after receiving their results, to better advise patients on what their LFD test result means.
Previous research into LFDs shows a range of estimates for sensitivity and specificity in different contexts of use. In the ‘BMJ practice pointer’, researchers explain that test characteristics (sensitivity and specificity) alone are of limited value in interpreting the test result. Knowing the pre-test probability, or the underlying likelihood of an individual having COVID-19 (eg, contact with a known case or link to an outbreak), is vital for interpreting the test result. When the disease incidence is low, a positive result should be validated by a polymerase chain reaction (PCR) test. However, if a clinician’s opinion is that COVID-19 is likely, then a positive test is likely to be reliable.
LFD testing is not recommended when the person has symptoms of COVID-19, as a negative LFD is not sufficient to rule it out. If a symptomatic patient informs their doctor that they have had a negative COVID-19 test, the clinician should check what type of test was carried out. If the clinician suspects COVID-19, a PCR test is recommended, even if the patient has received a negative result from a recent LFD test.
The researchers recommend clinicians ask about why the LFD test was done, as well as other factors that might influence underlying risk of COVID-19, including:
- Vaccination status
- History of previous infection
- A good understanding of the local epidemiology can improve interpretation. Local UK data is available at https://coronavirus.data.gov.uk/
- Also consider the quality of the testing (eg, who did the test, their familiarity with testing, and whether they used a recognised test). The sensitivity and possibly the specificity may decline if the quality of testing is weaker.
A source of concern with LFDs is that people might interpret a negative result as a “green light” and stop or reduce other protective behaviours. If this attitude is widespread, the benefits of testing, in terms of identifying cases and preventing transmission, could be offset by people relaxing effective measures that stop spread. The terms “red light” to describe a positive result (ie, stop all activities and isolate immediately) and “orange light” to describe a negative test (ie, continue to proceed with caution) may be helpful means to guide people’s behaviour.
Dr Jessica Watson, a GP and co-author of the practice pointer and National Institute for Health and Care Research (NIHR) Research Fellow at the University of Bristol’s Centre for Academic Primary Care and Applied Research Collaboration (ARC) West, said:
“The risks and benefits of using LFDs for widespread testing of asymptomatic people are the subject of ongoing uncertainty and debate. There is concern around LFDs relating to their ability to correctly pick up cases of SARS-CoV-2 infection, particularly when deployed in home and community testing.
“Distilling the complexity and uncertainty surrounding test results is not easy. We suggest that when sharing information about LFDs with the public it is best to be open, share uncertainty, and avoiding oversimplifying. In support of this approach, a recent trial found that wording that incorporated uncertainty around SARS-CoV-2 PCR tests led to fewer people interpreting results as definitive, and more people taking a cautious behavioural interpretation, for example continued self-isolation if symptomatic with a negative test.”
Dr Oliver Mytton, one of the authors added:
“It is really important to consider the clinical context when interpreting lateral flow tests. When somebody is likely to have COVID-19, a negative LFD test is not sufficient to rule out the disease, and a PCR test should be done. If the clinical assessment suggests that somebody is likely to have COVID-19, then a positive test is likely to be reliable and people should act accordingly.”
The calculator with this article uses sensitivity, specificity, and pre-test probability to estimate the likelihood that someone with a positive test actually has the infection. It can also be used to estimate other factors: the negative predictive value (the likelihood that someone with a negative test does not have the infection), as well as the likelihood of having a false positive or a false negative.
Paper