Coronavirus: how accurate are coronavirus tests?
17 April 2020
This blog, originally published by The Conversation, is by Dr Jessica Watson and ARC West alumna Associate Professor Penny Whiting.
Coronavirus testing has been the subject of huge interest, frustration and confusion. The UK has come under worldwide criticism for its lack of mass testing, despite the director general of WHO encouraging countries to “test, test, test”. Health Secretary Matt Hancock announced that the UK now aims to test 100,000 people a day for COVID-19 by the end of April.
There are two main types of COVID-19 tests. Swab tests, which usually take a sample from the throat or nose, to detect viral RNA. These determine if you currently have COVID-19. Blood tests, which detect antibodies, can determine if you have had COVID-19, and are therefore immune.
No test is 100% accurate. Although tests can perform well in ideal laboratory conditions, in real life lots of other factors affect accuracy including the timing of the test, how the swab was taken, and the handling of the specimen.
Early on in the novel coronavirus outbreak, doctors started reporting cases of people who had coronavirus which had been missed by swab tests – also known as “false negatives”. We don’t know for sure how often these false negatives occur in the UK, but evidence from China suggests up to 30 out of every 100 people with coronavirus might test negative.
The meaning of a test result for an person depends not only on the accuracy of the test, but also on the estimated risk of disease before testing. This was described mathematically by Thomas Bayes and later explained by Siddhartha Mukherjee as the law that “a strong intuition is much more powerful than a weak test”.
Let’s explain this with an example. Jane works for the NHS as a receptionist in a GP surgery in London, in an area of high rates of coronavirus infection. After noticing a loss of smell for a few days, she wakes up one night feeling shivery, with a dry cough. She checks her temperature to see it’s 38.5°C. However, after getting a swab test, the result comes back negative for COVID-19. Great news. Or is it?
Doctors use their experience to recognise patterns in symptoms, risk factors, and signs to estimate the likelihood of infection before testing. This is known as “pre-test probability”. Based on her symptoms, the probability that Jane has COVID-19 will be high – perhaps 80%.
However, let’s say 100 people experiencing symptoms like Jane have a swab test. Of these people, 80 actually have COVID-19. A positive test means we can be pretty certain someone has COVID-19. But if the test misses 30% of those 80 people with COVID-19, this means an estimated 24 out of 100 people will have a “false negative” test result. This means these people might go back to work and unknowingly spread coronavirus to others.
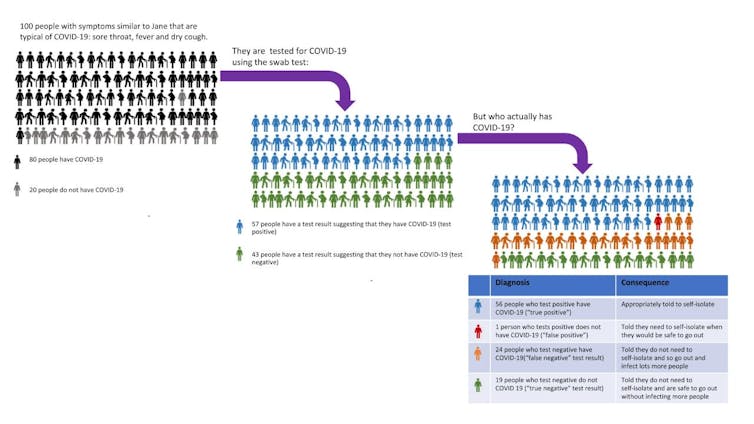
Jessica Watson/ Penny Whiting, Author provided
These numbers change depending on who is tested. If we test people with fewer symptoms, the likelihood of coronavirus or “pre-test probability” is lower. If only ten in 100 people tested actually have COVID-19, and 30% are missed by the test, this will mean only three in 100 people tested will have a “false negative”, compared to 86 “true negatives”. So if you have fewer symptoms and test negative, you can be more assured you don’t actually have COVID-19. But if you have typical symptoms of coronavirus, then it’s safest to assume that you have the disease, even if your test is negative.
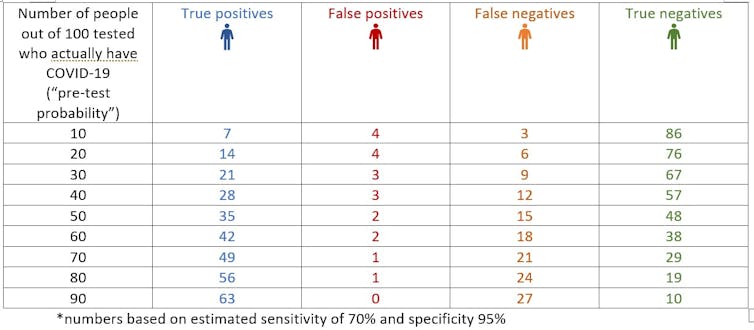
Jessica Watson/ Penny Whiting, Author provided
Antibody blood tests are also being developed. These could help us find out who has had coronavirus previously and is therefore presumed to be immune. This could help inform decisions about lifting lockdowns to allow people to go back to work safely.
But before these are rolled out, we need to know how accurate they are. This time we need to be confident that the antibody test doesn’t falsely reassure people that they are immune, as this could worsen the spread of infection. At the moment we don’t have enough information on these tests to be able to answer these questions. The very limited data available suggests they have fewer false negative results than swab tests, but more false positive results. This means there is a possibility that you could test positive without being immune and so these tests may not be as helpful as people are hoping.
The take home message is that testing is important to help understand and control the coronavirus outbreak – but it has limitations when used to guide decision-making for people. If you have strong symptoms of COVID-19, you should assume you have it – even if your test is negative.![]()
Jessica Watson, GP and NIHR Doctoral Senior Clinical Research Fellow, University of Bristol and Penny Whiting, Associate Professor in Clinical Epidemiology, University of Bristol
This article is republished from The Conversation under a Creative Commons license. Read the original article.